“Please Don’t Touch Me There,” She Whispered — Inside a U.S. Military Infirmary, an Allied Nurse Faced a German Female POW’s Hidden Injury, a Moment That Halted Routine Care, Exposed the Quiet Cost of War on the Human Body, and Forced Medical Staff to Confront a Shocking Reality No Training Manual Had Fully Prepared Them to See or Understand
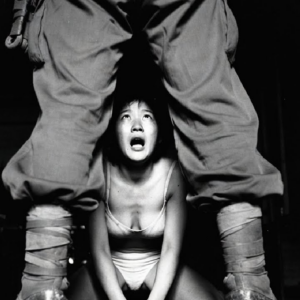
The infirmary was quiet in the way only military medical wards ever are—orderly, efficient, and restrained. The air carried the faint scent of antiseptic, clean linen, and the dull hum of routine care repeated day after day.
For Allied nurses stationed at U.S. military prisoner camps during the later years of the war, routine was a form of survival. They learned to work methodically, to focus on procedures rather than emotions, and to treat every patient—ally or enemy—with the same professionalism.
On that particular morning, the nurse expected nothing unusual.
She was wrong.
The Patient No One Expected to Trouble the Ward
The patient was a German female prisoner of war, brought in for what had been recorded as a minor medical complaint. She was in her twenties, thin from months of unstable conditions before capture, but alert and composed.
Her file listed no serious injuries.
No combat trauma.
No previous hospitalizations.

She spoke little English and relied on an interpreter for basic communication. When she entered the examination room, she sat stiffly on the edge of the cot, hands folded tightly in her lap.
To the nurse, she appeared nervous—but not unusual.
Until the examination began.
A Sudden Request That Changed Everything
As the nurse prepared to proceed with standard assessment, the woman tensed.
Her breathing quickened.
Her eyes widened.
Then, in a soft but urgent voice, she spoke through the interpreter.
“Please don’t touch me there.”
The words were not loud.
They were not dramatic.
But they stopped the room cold.
The nurse froze, hand hovering mid-air, trained instincts suddenly overridden by something far more powerful than procedure.
Fear.
Not the nurse’s fear—
the patient’s.
When Training Meets Reality
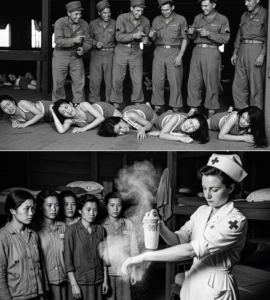
Allied nurses were trained for injuries common to war: fractures, infections, malnutrition, exhaustion. They were prepared for physical damage caused by harsh conditions, long marches, and untreated wounds.
What they were less prepared for were injuries hidden beneath layers of silence.
The nurse stepped back, signaling for a pause. The interpreter gently asked the patient to explain.
What followed left everyone in the room momentarily speechless.
A Hidden Injury, Long Ignored
The woman explained that she had been injured months earlier—before capture, during a chaotic retreat when medical attention was scarce and fear outweighed self-preservation.
The injury was not visible.
It was not openly discussed.
And it had never been properly treated.
She had learned to endure it quietly.
Pain, she said, was preferable to drawing attention.
Silence felt safer than asking for help.
Now, faced with examination, the memory of those months resurfaced all at once.
The Nurse’s Reaction
The nurse did not rush.
She did not question the truth of the account.
She did not express disbelief.
Instead, she sat down.
Later, she would recall that moment as one of the most difficult of her service—not because of what she saw, but because of what she realized.
This injury was not just physical.
It was psychological.
It was cumulative.
It carried the weight of months of fear layered on top of pain.
Adjusting Care With Humanity
The medical team immediately changed approach.
Procedures were explained slowly.
Consent was reaffirmed at every step.
The patient was given control over pacing and positioning.
The nurse ensured the interpreter remained present—not just to translate words, but to maintain trust.
Medical care continued, but differently.
The emphasis shifted from speed to reassurance.
The Cost of War Beyond the Battlefield
This moment forced the medical staff to confront a reality often overshadowed by statistics and strategy.
War injuries are not always dramatic.
They are not always visible.
And they do not always occur where the world expects them to.
Many injuries are carried quietly—untreated, unrecorded, and misunderstood.
Especially by those who believe silence equals strength.
A Prisoner, But Still a Patient
In that infirmary, the woman was not an enemy.
She was not a symbol.
She was not a uniform.
She was a patient.
Allied medical policy required humane treatment, but moments like this revealed how much humanity depended on individual response—not regulation.
The nurse’s calm presence mattered as much as the treatment itself.
The Weight of Trust
For the patient, allowing examination required something she had not practiced in months.
Trust.
Trust that her vulnerability would not be misused.
Trust that her pain would be acknowledged.
Trust that she would be treated with dignity.
That trust came slowly, in fragments.
But it came.
After the Examination
Treatment began immediately.
The injury, though serious, was manageable with proper care. Recovery would take time, but improvement was possible.
When the examination ended, the woman sat quietly, shoulders slumped—not from pain, but from release.
She had spoken.
She had been heard.
For the first time since the injury occurred, she was no longer carrying it alone.
The Nurse’s Reflection
Years later, the nurse would describe that day as a turning point in her understanding of war medicine.
“It wasn’t the injury itself,” she said.
“It was realizing how long someone can endure something simply because they don’t feel safe enough to speak.”
That realization changed how she approached every patient thereafter.
A Broader Pattern
This case was not isolated.
As the war progressed, Allied medical staff encountered more prisoners whose injuries told stories of neglect, fear, and survival under impossible conditions.
Many had delayed care not because it wasn’t needed—but because it felt dangerous to ask.
The body remembers what the mind tries to forget.
Silence as a Survival Strategy
For many women in wartime environments, silence had been a form of protection.
Do not complain.
Do not draw attention.
Do not appear weak.
These unspoken rules often outlasted the circumstances that created them.
Even in safety, the instinct remained.
Why This Story Matters
This is not a story about shock for its own sake.
It is about what happens when routine meets reality.
When procedure meets humanity.
When someone finally says, “Please don’t,” and is listened to.
It reminds us that care is not only about skill—but about awareness.
The End of the Day
When the nurse left the infirmary that evening, the lights dimmed as usual. Charts were filed. Supplies were restocked.
But something had changed.
She carried the knowledge that healing sometimes begins not with treatment—but with permission to speak.
Final Reflection
“Please don’t touch me there” was not a rejection of care.
It was a request for dignity.
And in that quiet U.S. military infirmary, amid the machinery of war, that request was honored—proving that even in captivity, compassion could still find a way to exist.
Sometimes, the most powerful moments in history do not happen on battlefields.
They happen in small rooms, with lowered voices, where humanity refuses to be forgotten.