He Expected Routine Checkups—Instead an American Army Doctor Uncovered a Silent Crisis Among German Women Prisoners, Faced an Emotional Breaking Point, Made a Risky Medical Call Against the Clock, and Triggered a Chain of Decisions That Quietly Prevented a Tragedy No One Else Had Seen Coming
A Medical Assignment Meant to Be Ordinary
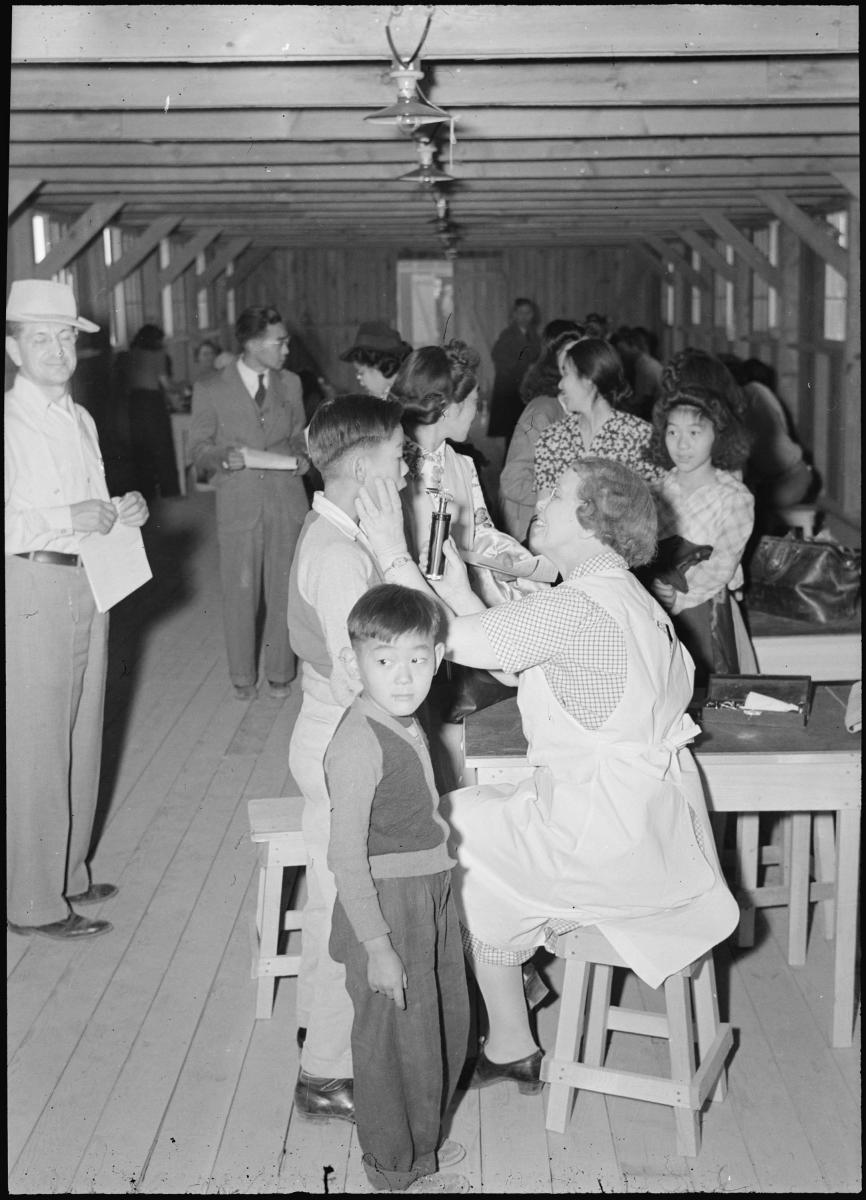
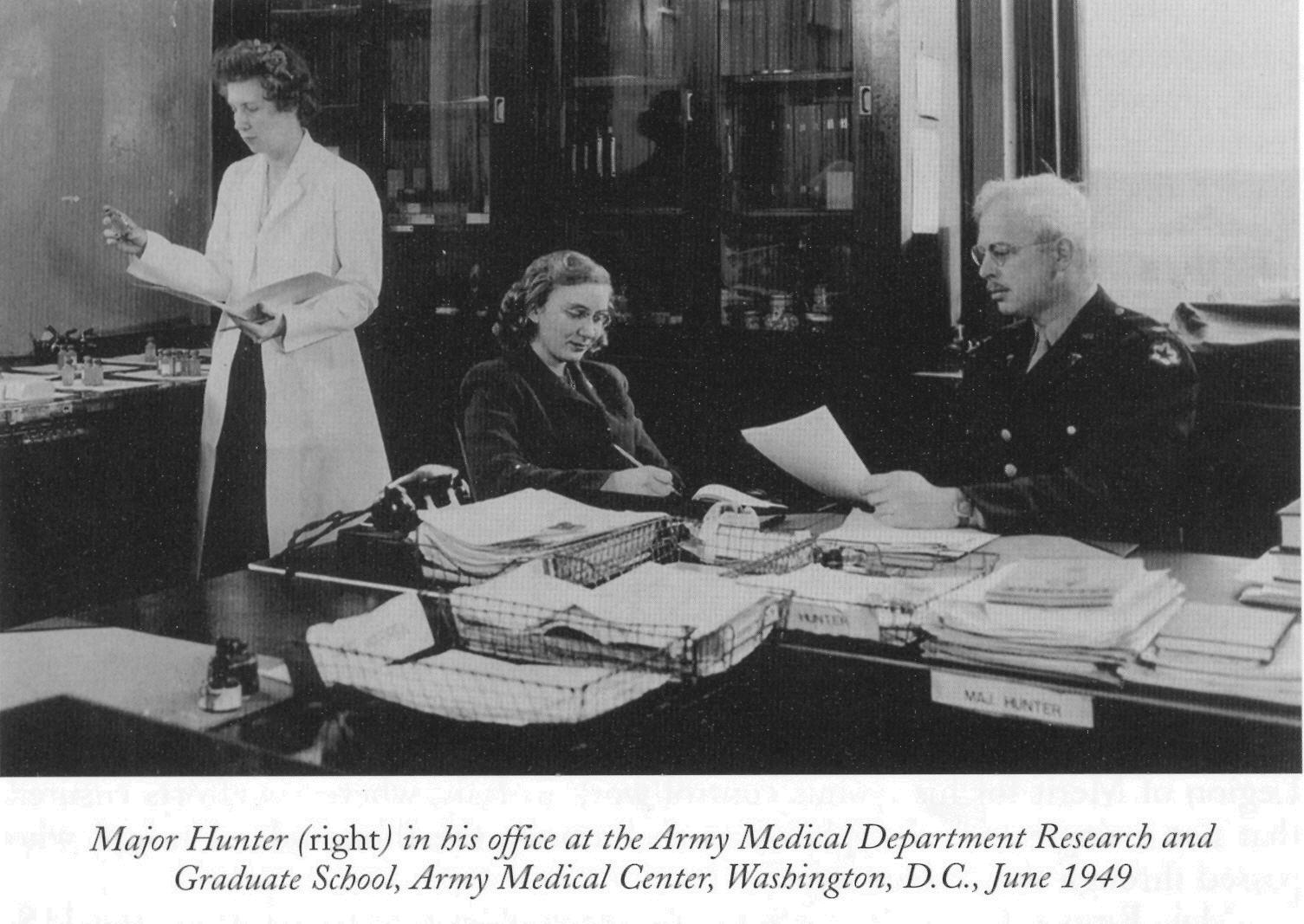
In the later years of the Second World War, medical officers in American custody camps were accustomed to routine. Examinations followed schedules. Paperwork followed procedure. Patients—whether soldiers or prisoners—were assessed, treated, and documented with efficiency shaped by necessity.
When an American military doctor was assigned to conduct health evaluations of German women prisoners of war, there was no indication that this task would be any different. The assignment was framed as standard protocol: assess general condition, identify communicable risks, and clear individuals for continued detention or transfer.
Nothing in the briefing suggested urgency.
Nothing warned him that what he was about to encounter would challenge his composure, his assumptions, and his understanding of how close quiet systems can come to collapse.
The First Signs That Something Was Wrong
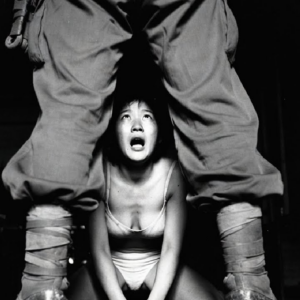
The examinations began as expected. Basic measurements. Visual assessments. Questions translated and answered politely, if cautiously. The women appeared orderly, composed, and compliant.
But patterns began to emerge.
One patient showed extreme fatigue inconsistent with her age. Another had unexplained swelling. Several displayed similar symptoms that, taken alone, might have been dismissed as stress or malnutrition. Taken together, they formed a troubling picture.
The doctor paused.
War teaches medical professionals to move quickly, but also to notice repetition. And repetition, in medicine, is rarely accidental.
A Growing Unease
As examinations continued, the unease grew. The women were not complaining openly. Many minimized their discomfort. Some struggled to articulate symptoms across language barriers. Others simply endured silently.
Yet the signs were there—subtle, but consistent.
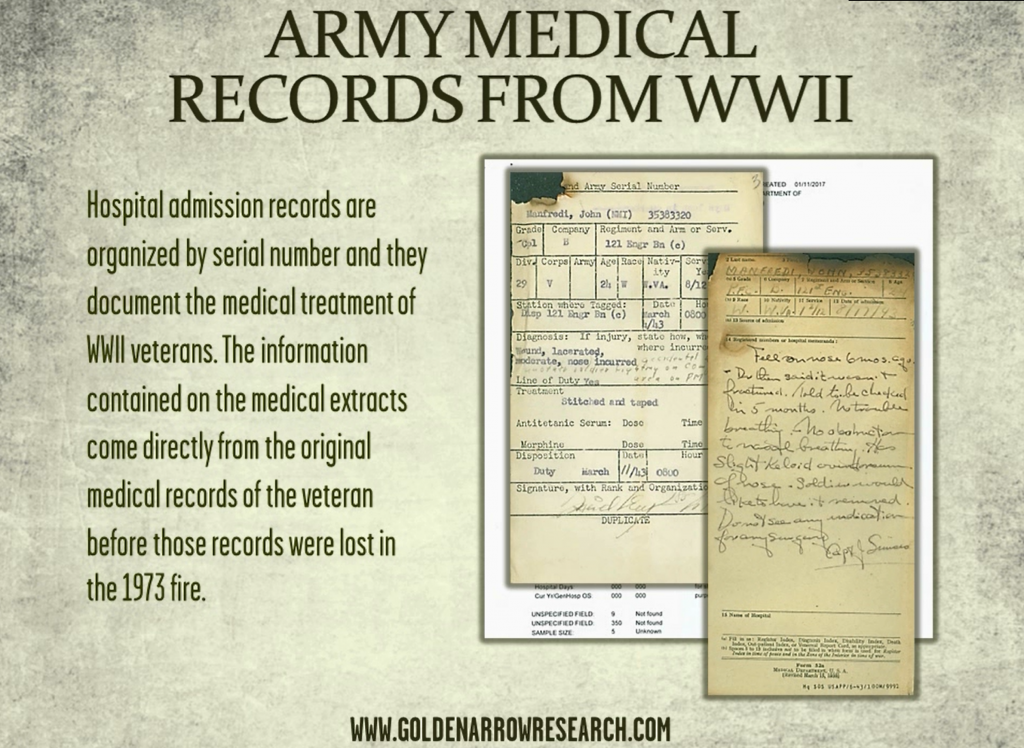
The doctor began reviewing notes more carefully. He compared charts. He recalculated timelines. What he saw did not align with the assumption that these were isolated cases.
This was something broader.
And it was being missed.
The Emotional Breaking Point
The realization did not arrive dramatically. There was no sudden outburst, no collapse in front of others. Instead, the weight accumulated quietly.
At one point, reviewing records late into the night, the doctor stopped writing.
He understood what the data suggested.
A condition—preventable, treatable if caught in time—was spreading unnoticed among the women. Left unaddressed, it would worsen rapidly. Not violently. Not suddenly.
Silently.
That was the most dangerous part.
The doctor later described this moment as the hardest of his service. Not because of graphic injury or battlefield chaos, but because of what it represented: lives at risk due to invisibility.
The Hidden Factors
Several elements had contributed to the situation.
The women came from different units, backgrounds, and regions. Their shared symptoms were easy to overlook amid wartime stress. Nutritional deficiencies, prolonged strain, disrupted routines, and delayed reporting all played a role.
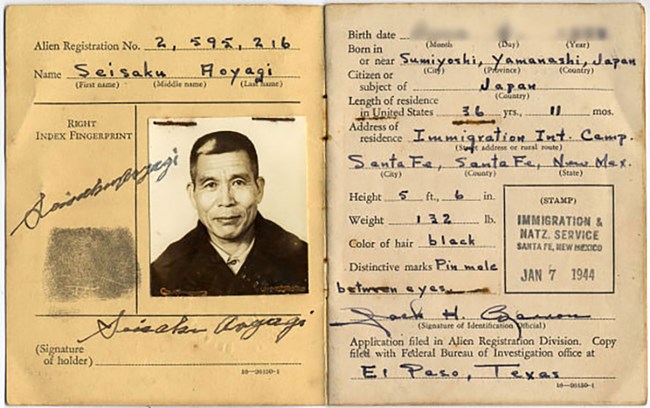
Additionally, assumptions worked against them. Because they were not combat troops, their medical evaluations were less frequent. Because they were orderly, their silence was mistaken for stability.
And because resources were stretched, subtle warnings went unprioritized.
Until now.
Choosing to Act
The doctor faced a choice.
He could document findings and follow standard timelines, trusting the system to respond eventually. Or he could escalate immediately, pushing for intervention that would disrupt routines, require resources, and draw attention.
He chose the latter.
This decision was not without risk. Wartime systems value efficiency. Questioning assumptions invites scrutiny. But medical ethics leave little room for hesitation when lives are involved.
He submitted an urgent report. He requested additional supplies. He recommended immediate treatment protocols and closer monitoring.
And then he waited.
Resistance and Delay
Initial responses were cautious. Requests for additional resources during wartime were common—and often denied. Administrators questioned whether the issue was as widespread as suggested.
The doctor persisted.
He provided data. He showed patterns. He explained consequences without exaggeration.
His insistence was not emotional. It was precise.
That precision made the difference.
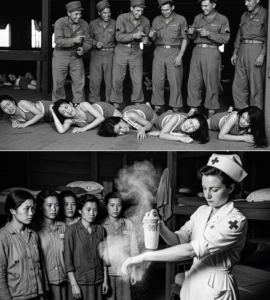
The Intervention Begins
Approval came quietly.
Treatment protocols were adjusted. Diets were supplemented. Rest periods were enforced. Follow-up examinations became mandatory rather than optional.
The changes did not look dramatic from the outside. No emergency alarms. No mass evacuations.
But inside the camp, the effect was immediate.
Symptoms stabilized. Recovery began. Complications were avoided.
By the time the full scope was understood, the estimate was clear: at least forty women had been spared serious, potentially fatal outcomes.
Lives Saved Without Headlines
There were no announcements. No medals. No official ceremonies.
The women returned to routine. The camp resumed its rhythm. Records were filed.
Yet something irreversible had occurred.
A crisis that never became visible had been prevented entirely. And prevention, by nature, leaves no dramatic evidence behind.
The Doctor’s Private Reckoning
For the doctor, the experience left a lasting mark. He did not speak of it often. When he did, he emphasized not heroism, but fragility.
Systems, he explained, are only as effective as their willingness to notice the quiet cases.
The emotional breaking point he experienced was not weakness. It was recognition—of responsibility, of consequence, of the cost of overlooking those who do not shout for help.
The Women Who Never Knew the Full Story
Most of the women never learned how close they came to severe outcomes. They knew treatment had improved. They felt stronger. Life continued.
That ignorance was intentional.
The goal was not to frighten, but to heal.
In many ways, that quiet normalcy was the greatest success.
Why This Story Stayed Hidden
Stories like this rarely surface in historical narratives. They lack spectacle. They resist simplification. They do not fit easily into tales of victory or defeat.
They exist in margins—in medical logs, in personal memory, in outcomes that never occurred.
Yet they reveal something essential about wartime humanity.
Beyond National Lines
The doctor did not act because the patients were German. He acted because they were human.
This distinction mattered.
Medical ethics, even in war, recognize no uniform. The obligation to prevent harm does not disappear when borders change.
In choosing to see individuals rather than categories, the doctor upheld a principle that often goes uncelebrated but remains foundational.
The Cost of Silence
The episode also highlights a dangerous truth: silence can be misinterpreted as resilience.
The women endured discomfort without complaint. Cultural expectations, fear, and discipline all contributed. Their silence nearly cost them everything.
It took attentive observation—not dramatic symptoms—to uncover the risk.
A Lesson That Outlived the War
Years later, the doctor reflected that the most important skill he used that day was not technical expertise, but attention.
Noticing patterns. Questioning assumptions. Acting before proof became tragedy.
These lessons extended beyond war.
Why This Still Matters Today
Modern systems still struggle with invisible crises. Overlooked groups. Subtle warnings dismissed as anomalies.
This story reminds us that prevention rarely looks heroic—but it saves lives nonetheless.
Forty Lives, Quietly Preserved
No monument marks the moment. No plaque records the decision.
But forty women lived because one doctor refused to accept “routine” as an answer.
The Unseen Victory
War is often measured by territory gained or lost. Yet sometimes its most meaningful victories occur far from battlefields—in examination rooms, in late-night reviews, in decisions made by individuals who choose responsibility over convenience.
An American doctor broke down—not from weakness, but from clarity.
And because he did, forty lives continued forward—untouched by a tragedy that never had the chance to happen.