An American Doctor Examined German POW Women Expecting Routine Fatigue—What He Discovered Instead Shocked the Camp, Exposed a Silent Crisis Hidden in Plain Sight, and Triggered Urgent Changes That Quietly Saved Forty Lives Before It Was Too Late
In the late stages of World War II, medical inspections inside prisoner-of-war camps were meant to be predictable.
They followed checklists.
They focused on numbers.
They existed to keep systems running.
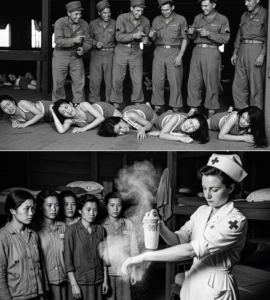
When an American military doctor was assigned to examine a group of German women held as POWs at a temporary camp, no one expected the visit to become memorable. The women had already been processed, counted, and categorized. Supplies were limited, schedules were tight, and attention was focused elsewhere.
This inspection was supposed to take an hour.
It changed everything.
The Camp at a Crossroads
By the time the doctor arrived, the camp was in transition. Front lines had shifted. Personnel rotated frequently. Temporary facilities were being used far longer than intended.
The women—around forty in total—had arrived weeks earlier as part of a larger transfer. They were not combatants. Most had been attached to wartime labor units, clerical roles, or had been displaced during rapid territorial changes.

They were quiet.
They followed instructions.
They did not complain.
To camp administrators, that meant “no problem.”
To the doctor, it meant something else entirely.
The First Signs Something Was Wrong
The doctor began as he always did: observation before examination.
He noticed posture first.
The women stood carefully, as if conserving energy. Movements were deliberate. Faces were composed, but eyes avoided prolonged contact—not out of fear, but exhaustion.
This wasn’t dramatic.
It was subtle.
And subtle patterns are often the most dangerous.
When Experience Overrides Assumptions
The doctor had seen fatigue before.
He had treated soldiers fresh from marches, civilians displaced by bombardment, and detainees weakened by months of uncertainty. What he saw here did not match typical exhaustion.
The symptoms didn’t align.
Breathing was shallow.
Skin tone varied inconsistently.
Responses to simple questions lagged.
Individually, each sign could be dismissed.
Together, they formed a picture he couldn’t ignore.
“How Long Has This Been Happening?”
The doctor asked a question through an interpreter.
“How long have you felt like this?”
The answers were vague.
“Some time.”
“Since before arriving.”
“It comes and goes.”
None of the women wanted attention. Several actively minimized their condition, insisting they were fine.
That concerned him more than if they had complained.
The Quiet Danger of Being Overlooked
In wartime systems, silence is often misread as stability.
The women had adapted to scarcity by rationing themselves—food, movement, even expression. They did not want to stand out. They did not want to delay transfers or attract scrutiny.
This adaptation, while understandable, had masked a growing problem.
One that standard procedures were not catching.
The Examination That Changed the Timeline
As the doctor moved from observation to examination, inconsistencies multiplied.
Vital signs fluctuated unexpectedly.
Muscle weakness appeared disproportionate to intake records.
Cognitive fog was present in women of different ages and backgrounds.
These were not isolated cases.
This was a pattern.
And patterns save lives when someone recognizes them in time.
The Truth Hidden in Logistics
The doctor reviewed camp records closely.
On paper, the women were receiving adequate rations.
Water access was listed as sufficient.
Rest periods were documented.
But paperwork doesn’t capture reality.
He cross-checked delivery logs with distribution schedules and realized something critical: timing and composition were mismatched. Nutritional balance had been assumed, not verified.
The camp was following procedure.
The procedure was wrong.
Why Forty Lives Were at Risk
The issue wasn’t one catastrophic failure.
It was accumulation.
Small deficits over time.
Minor shortages repeated daily.
Assumptions carried forward without reassessment.
In healthy populations, such deficits might be tolerable.
In stressed, displaced individuals, they are not.
The doctor understood that without intervention, the women would continue to decline—not dramatically, but steadily.
Quietly.
Pushing Against the System
Raising concerns inside a military structure is never simple—especially during active operations.
The doctor requested immediate changes.
Additional evaluations.
Adjusted intake.
Revised schedules.
Initial responses were cautious.
Resources were stretched.
Priorities were set.
Nothing seemed urgent enough.
So the doctor escalated.
Not emotionally.
Professionally.
He documented patterns, referenced precedent, and made one thing clear: delay would create an emergency that didn’t need to happen.
When Authority Listens to Evidence
The difference between being ignored and being heard often lies in preparation.
The doctor had it.
Within hours, camp leadership approved temporary changes.
Food composition was adjusted.
Rest periods were extended.
Medical follow-ups were scheduled regularly.
None of this made headlines.
But it changed outcomes.
The First Signs of Recovery
The effect was noticeable within days.
The women’s posture improved.
Speech became more responsive.
Fatigue lessened—not disappeared, but stabilized.
One woman asked for extra work detail, surprising guards accustomed to passivity.
Another laughed for the first time since arrival.
These were small indicators.
They meant everything.
Why the Discovery Shocked Everyone
What shocked camp personnel was not that the women were struggling.
It was how close the system had come to missing it entirely.
No alarms had sounded.
No collapse had occurred.
No crisis had announced itself.
Forty lives had been drifting toward a tipping point without a single dramatic signal.
The danger had been ordinary.
The Women Speak—Carefully
When asked later how they felt, many women struggled to answer.
Not because they lacked words.
Because they had learned not to use them.
They spoke of adapting.
Of not wanting to be “a problem.”
Of assuming this was simply how things were now.
The doctor recognized the pattern instantly.
Silence had become survival.
The Ethical Line That Matters
Military medicine is often framed as triage—deciding who needs help most, fastest.
But this case revealed something deeper.
Prevention saves more lives than reaction.
Listening saves more lives than force.
Reassessment saves more lives than assumption.
The doctor had not saved anyone with dramatic intervention.
He had saved them by noticing.
A Change That Outlasted the Camp
The adjustments made for the women were later applied to other groups passing through the camp.
Procedures were refined.
Schedules updated.
Assumptions questioned.
The system learned—quietly, without fanfare.
And that learning mattered far beyond this one place.
Why This Story Nearly Disappeared
There was no incident report titled “Forty Lives Saved.”
No ceremony.
No commendation.
From an administrative perspective, nothing had gone wrong.
From a human perspective, everything could have.
History tends to record failure loudly and success quietly—especially when success looks like nothing happening.
Lessons That Remain Relevant
This story matters because it challenges how we think about crisis.
We imagine danger as sudden and obvious.
We imagine rescue as dramatic.
In reality, danger often accumulates silently—and rescue often looks like a clipboard, a question, and the courage to insist on a second look.
Compassion Without Drama
The doctor never described his actions as heroic.
He described them as necessary.
He did not frame the women as victims.
He did not frame himself as a savior.
He framed the situation as incomplete—and acted accordingly.
That humility made the difference.
The Women Who Walked Away
When the women were eventually transferred, they left stronger than they had arrived.
Not unscarred.
Not untouched.
But alive.
Stable.
Capable of continuing.
Forty lives continued forward—not because of luck, but because someone took time to look closely.
Redefining What “Saving Lives” Means
Saving lives doesn’t always involve stopping something terrible.
Sometimes it means preventing something quiet.
It means noticing patterns before they escalate.
Correcting course before collapse.
Valuing human signals over bureaucratic comfort.
This doctor did all three.
Why the Truth Still Resonates
In modern systems—medical, institutional, corporate—the same risks exist.
People adapt.
People minimize.
Systems assume.
And lives depend on whether someone pauses long enough to ask, “Does this really add up?”
A Final Reflection
An American doctor entered a POW camp expecting routine fatigue and paperwork.
What he found instead was a silent crisis hiding in compliance.
By trusting experience over assumption and evidence over routine, he triggered changes that saved forty lives—without sirens, without headlines, and without recognition.
Sometimes, the most shocking truth isn’t that danger exists.
It’s how easily it can be missed—and how powerful it is when someone refuses to miss it.